Speech-Language Pathology
Speech-Language Pathologists (SLPs) at Easterseals strengthens children's communication and feeding skills so they can participate fully in daily activities and achieve success. Our SLPs addresses language comprehension, pragmatics, speech-sound production, voice, fluency, as well as oral motor and feeding skills. We offer a comprehensive, fun and engaging experience for children to learn and develop their skills. We pride ourselves in looking at the whole child and merge evidence-based therapies and a neurodiversity-affirming approach to positively impact the whole family.
To get started, contact us
Or our Admissions Supervisor by email or phone at 630.282.2022 to ask questions or for scheduling.
Click here to learn more about our Assistive Technology program with a focus on Augmentative and Alternative Communication (AAC) for individuals with complex communication needs.
Why Begin Here?
Not only do we offer creative and innovative services with our experienced and passionate therapists- we are committed to ensuring the success of each child. We value each family and celebrate together as goals are achieved.
Our clinicians are focused on continually advancing our skills and learning new techniques to fit the needs of the infants, children and adults we serve. Most speech-language sessions are one-on-one with a speech language pathologist, but we also offer parent coaching models, co-treatments with an occupational, physical or developmental therapist, tele-therapy services and group therapy sessions like our Fun with Foods group. We collaborate with other Easterseals, school and medical professionals to make sure a child's goals are reached in all environments.
Experts agree! We are a top CARF (Commission on Accreditation of Rehabilitation Facilities) accredited pediatric outpatient rehabilitation provider for more than 40 years and an NDTA- Center of Excellence since 2019.
Our speech-language pathologists also have specialized training in a variety of areas including:
- Apraxia of Speech
- Articulation
- Auditory & language Processing
- Executive Functioning
- Functional Communication/Early Language
- Feeding Challenges: G-tube/PEG tube Weaning, Oral Motor Feeding, Sensory Feeding
- Literacy: Spelling & Reading
- Narration: Oral & Written
- Phonology
- Receptive/Expressive Language
- Respiration
- Social-Pragmatic Language
- Stuttering
- Voice
Our expert speech-language pathologists hold certificates in:
- DIR Floortime
- Early Intervention Evaluators & Specialists
- Neurodevelopment treatment- NDT
- Sequential Oral Sensory Approach- SOS
Easterseals DuPage & Fox Valley has several specialty clinics, many that are interdisciplinary, that provide specific and individual care to best suit a child's needs. Speech-language pathologists serve on the below specialty clinics.
Technology
While advancing our skills, our therapists have honed techniques in our Voice Box: A Motor Speech Lab, which focuses on improving articulation, voice and resonance skills through cutting edge and innovative technology using a Smart Palate, Nasometer and Visipitch. We can also include SMARTBoards in sessions to promote interactive games that help teach new speech patterns.
We also have a premier Assitive Technology program that can help individuals with complex communication needs thrive with the right supports at school and home.
How Do I Get Started?
Contact our Intake Coordinator Diana Dixon at 630.282.2022 to ask questions or schedule an appointment.
Are you interested in learning more about our virtual services options? Click here to learn more about Tele-Therapy.
Programs
Our blog
-
Helping Children Ride a Bike
Thursday, June 12, 2025, 1:09 PM
By: Josephine Hipolito, PT, C/NDT Physical Therapist Summer is a popular time when caregivers ask me…
Read this PostBy: Josephine Hipolito, PT, C/NDT
Physical TherapistSummer is a popular time when caregivers ask me to work on bike riding with their kids as one of their goals. As an avid cyclist, it’s one of my favorite things to teach because of the joy and freedom children feel when they learn to ride. Let’s start with a few tips on teaching children bike riding.
How to Begin

- Determine whether the child knows how to pedal. If they do, skip the next section and go to the balance section to work on the balance aspect of bike riding .
- Remember you don’t have to follow this step by step. It’s more of a guide to see where your child is in the bike riding process and then proceed.
Teaching Children Pedaling:
- Start with teaching “Air Cycling.” Most kids don’t understand the concept of extending one leg while the opposite leg is relaxed if they have never pedaled before. Their usual instinct if you tell them to push with their legs is to have both legs push simultaneously, so they usually get stuck when on a tricycle.
- To practice the motion of pedaling, place your hands at the bottom of their feet and tell them to push against it on their bent leg. Use a little resistance when you do this. On a tricycle, kids often stop pedaling and move backward when they encounter resistance, so you want them to get used to resistance.

3. Once they master air cycling, start them on a tricycle with a pedal block (a device that holds their feet on the pedals) or strap their feet on the pedals using an ace wrap or velcro straps. Children usually tend to over-push with their feet at first, so their feet slip off the pedals. Wrapping their feet will keep them on the pedals. You can also get commercially available pedal straps like this one.
4. Once they master the pedal block, take off the straps so they can learn to control their leg movement and keep their feet on the pedals.
5. Make sure they master pedaling with a tricycle so that it becomes second nature to them when they graduate to a bicycle.

Balance Bike Versus a Bike with Training Wheels
I often tell families ready to progress their children from a tricycle to a bike, to start with a balance bike. A balance bike is simply a bike without pedals where children use their legs instead of pedals to move.
Skip the step of learning with training wheels because children can get dependent on leaning on them for balance. The Balance Bike enables the child to learn to find their center of balance on their own
NOTE: Not everyone will be able to get a balance bike and a bike with training wheels, so I recommend taking the training wheels AND the pedals off of a bike to convert it to a balance bike. A bike shop can help make this adjustment.
Biking with Training Wheels
The problem with a bike with training wheels is the braking system. They use coaster brakes which means pedaling backward to activate the brakes.
Kids tend to start pedaling backward when they encounter resistance which activates the brakes. It’s always difficult for kids with motor planning issues to figure this out. That’s why you ensure they master the pedaling part of bike riding before moving on.

Keep an eye out for the following:
- Some kids tend to push with their legs while pulling on the handlebars, which causes the bikes to turn – as a PT, this signals to me that they need core strengthening
- Some kids will over push with their legs causing them to slip backward on the bike seat – I put a dycem (non-slip pad) or tie a theraband on the seat to prevent this .
Tips to Use a Balance Bike
- Start with having the child walk with their legs while sitting on the saddle. See if they have the control to keep the bike from tipping or even recognize that the bike is tipped while they are riding it. They need to integrate this part. Children with body awareness issues will not even recognize that they are tilted when propelling a balance bike.
- Watch out for kids who walk the bikes, but they are standing and not sitting on the seat. I sometimes use an ace wrap to secure their pelvis on the seat to prevent this
- Once they master keeping the bike upright, work on gliding .
- Gliding – have them take three steps: 1, 2, 3, then bring their feet up to glide. Challenge them and ask them to see how far they can glide before they put their feet down.
- I sometimes use floor markings like chalk on the surface to mark a certain point. Children can work on balancing better if they have a visual cue on how far to glide.
- Once a child can glide for 10-20 feet consistently, I move them to a bike with two wheels (or put the pedals back on the bike).
Steps to Help Children Ride a Standard Bike
- Work in a parking lot of a school or a park early in the morning so that it will be empty and there are no distractions – avoid the sidewalks or narrow spaces because the child tends to worry about staying within the confines of the space (it can become too stressful for them).
- Try to find a parking lot with a little downward incline to help them get a little momentum to balance.
- Let your child walk the bike out to the parking lot while holding the handlebar. This way, they learn to handle the bike and how to motor plan to keep it balanced.
- Work on pedaling forward first. Worry about turns later.
- Have a gait belt (or a man’s belt) around their trunk, so you have something to grab onto when they are riding (if they are not using a bike with a parent’s handle).
- Give them a little push to start them up – they will usually start slow because they are apprehensive but what children don’t realize yet is they need momentum to be able to balance.
- Give them frequent breaks, and bring a snack, as bike riding can be stressful while learning. Let them know that they have to do 2-3 laps then they can take a break. Break for 1-2 mins, get a drink or snacks, then return to bike riding. Use a timer so they know break time is over when it rings. This way, they may be more cooperative when they know they have a break.
- Once they master going straight, you can work on turning – put cones on each end of the parking lot and ask them to turn around the cones. This way, they can practice tight turns.
- Once they master turning, work on tighter areas (e.g. a hallway, sidewalk) to narrow their space.
- Once they master tight areas, work on going up inclines.
Biking From a Complete Stop
- Determine the child’s balance leg – it’s usually the first leg they put down when they stop.
- Once that’s determined, the balance leg is the leg that will stay on the ground and will be pushing to get the bike going. The other leg goes on the pedal (pedal leg).
- Teach the child to position the pedal (pedal leg side) in front of their shin so they can easily put their foot on it.
- Ask them to have the balance leg push on the ground while the pedal leg is pushing down on the pedal to start the bike .

Cycling Benefits
I hope this blog has been helpful wherever your child is on their cycling journey! Teaching children to cycle has numerous benefits to their development, including improving motor skills, strength and balance. It’s also a fun exercise that can be enjoyed with a sibling, a neighbor, or friend!
If you ever have concerns about your child’s mobility, strength, or motor skills, Easterseals DuPage & Fox Valley is here to help! Learn more about our physical therapy services by visiting:
https://www.easterseals.com/dfv/our-programs/medical-rehabilitation/physical-therapy.We also invite your family to join our annual Bike for the Kids in Elgin on August 24, 2025!
Hop on the bike trail system of your choice and meet up in South Elgin for a 10th Anniversary Festival recognizing the cycling and wheeled achievements of children at Easterseals DuPage & Fox Valley. Whether you ride from near or far, you represent a community served by Easterseals.

Opportunities to join also include a guided cycling ride, a play date at SEBA park, and our 10th Anniversary Festival. Featuring live music, a kid zone, food, and games, there will be lots of fun for kids who thrive on bikes, trikes, scooters, trailers, and wheelchairs.

Learn more and register here:
https://secure.qgiv.com/event/bikeforthekids25/ -
Paging Dr. Play: Pediatric Medical Procedure Support at Easterseals
Wednesday, September 18, 2024, 10:59 AMPaging Dr. Play: Pediatric Medical Procedure Support at Easterseals
Wednesday, September 18, 2024, 10:59 AM
By: Katelyn Bentel, MSW, LSW Medical-related appointments can elicit feelings of worry/anxiety, whet…
Read this PostBy: Katelyn Bentel, MSW, LSW
Medical-related appointments can elicit feelings of worry/anxiety, whether it is a routine wellness check-up, blood draw, or a surgery requiring a hospital admission. As an adult, we can understand how the benefits of going through these medical encounters can outweigh the discomfort of the anticipatory anxiety.
However, a child developmentally is not as able to rationalize the need or benefit of undergoing these medical experiences. The child also may not have the skill to work through their emotions regarding the procedure. The way children can strengthen these developmentally appropriate, social-emotional skills is through play.
Philosopher, Jean Jaques Rosseau stated, “Play is the universal language of childhood. It is through play that children understand each other and make sense of the world around them.”
Medical play is a great way to help a child prepare for an upcoming appointment or procedure; especially if there is a history of medical trauma, heightened emotions during medical-related appointments, and/or the caregiver anticipates that the child will experience emotional distress.
By providing opportunities for children to play out upcoming events and gain exposure to equipment that is found in medical environments, they can begin to feel a sense of control and experience lower levels of anxiety.
Medical Procedure Support Service at Easterseals DuPage & Fox Valley
Easterseals DuPage & Fox Valley now offers Medical Procedure Support services and recommendations led by a social worker to help ease a child’s worry, distress or discomfort.
This program involves 4 sessions, consisting of:
- Initial parent or caregiver evaluation with a social worker
- 2 pre-procedure support sessions with the child and their caregiver
- Post-procedure processing session with the child and their caregiver
In the intake process or initial caregiver evaluation, we can discuss the best timing for your child and family. This service can also include support before dental appointments, vaccinations and other procedures that can cause anxiety for children and their caregiver.
What Does Medical Play Look Like?

Bronchoscopy - Creating art with medical equipment (e.g., Band-Aids, syringes, gauze/cotton balls, anesthesia masks, tongue depressors, medical gloves, pill bottles, etc.)

- Role playing with dolls and medical kits (e.g., doctor & dentist)
- Reading developmentally appropriate books/social stories or watching videos about medical procedures
- Making diagrams/models (e.g., drawings, clay, etc.) of specific body parts
By playfully interacting with medical equipment, children can become desensitized to the objects—meaning that the equipment becomes less intimidating because it is familiar to the child and has been used in a non-threatening manner.
Additionally, a child and caregiver/therapist can take on different roles in medical play to normalize various emotions and determine coping strategies that feel more supportive for that individual. We all have different preferences (e.g., deep breathing, distractions, being verbally walked through each step, physical touch, etc.)!
Utilizing Play During Medical Procedures
Medical play also allows for children to explore, identify, and practice coping strategies that can be utilized during appointments/procedures. For example, blowing bubbles through an anesthesia mask is a way to practice deep breathing.

If a child is scheduled for a blood draw, here are potential opportunities that can be implemented to give some control back to the child before, during, and/or after the blood draw:
- Before: picking who will accompany them, which toy/fidget they will bring for support, etc.
- During: picking which arm (if possible), choosing if they want to look/watch, choosing if they want to be sitting on a caregiver’s lap, if they want their hand held, choosing if would they like a distraction (e.g., picture seek-and-find, video), etc.
- After: Getting to pick something enjoyable to do once the procedure is complete, such as going to the park, getting a special snack/treat, having a movie/game night at home, etc.
Supporting Children’s Overall Health
Though the medical world can be intimidating and scary for children and adults at times, it is also a key factor for supporting overall health. Nobody wants to be sick or need medical intervention, but it is a part of life that can be out of our control.
Medical play is that opportunity for children to lessen their anxiety and ease the medical experiences to meet their health needs! If an anticipated, distressing medical appointment/procedure is approaching, it is time to page Dr. Play and “scrub in!”
Please note that we are not affiliated with a specific hospital system and encourage you to consult your doctor for education and guidance surrounding your child’s appointment.
For more information, please contact, Director of Mental Health and Family Support, Brittany Wilkie, LCSW at 630.261.6272 or bwilkie@eastersealsdfvr.org.
To schedule services, please contact Michele Tabachka at mtabachka@eastersealsdfvr.org or 630.282.2023.
-
It’s Summer! Let’s Go Ride A Bike!
Monday, July 29, 2024, 10:32 AM
By: Josephine Hipolito, Physical Therapist Summer is a popular time when caregivers ask me to work o…
Read this PostBy: Josephine Hipolito, Physical Therapist
Summer is a popular time when caregivers ask me to work on bike riding with their kids as one of their goals. As an avid cyclist, it’s one of my favorite things to teach because of the joy and freedom children feel when they learn to ride. Let’s start with a few tips on teaching children bike riding.
Things to Consider When Starting

- Determine whether the child knows how to pedal. If they do, skip the next section and go to the balance section to work on the balance aspect of bike riding .
- Remember you don’t have to follow this step by step. It’s more of a guide to see where your child is in the bike riding process and then proceed.
Teaching Children Pedaling:
- Start with teaching “Air Cycling.” Most kids don’t understand the concept of extending one leg while the opposite leg is relaxed if they have never pedaled before. Their usual instinct if you tell them to push with their legs is to have both legs push simultaneously, so they usually get stuck when on a tricycle.
- To practice the motion of pedaling, place your hands at the bottom of their feet and tell them to push against it on their bent leg. Use a little resistance when you do this. On a tricycle, kids often stop pedaling and move backward when they encounter resistance, so you want them to get used to resistance.

3. Once they master air cycling, start them on a tricycle with a pedal block (a device that holds their feet on the pedals) or strap their feet on the pedals using an ace wrap or velcro straps. Children usually tend to over-push with their feet at first, so their feet slip off the pedals. Wrapping their feet will keep them on the pedals. You can also get commercially available pedal straps like this one.
4. Once they master the pedal block, take off the straps so they can learn to control their leg movement and keep their feet on the pedals.
5. Make sure they master pedaling with a tricycle so that it becomes second nature to them when they graduate to a bicycle.

Balance Bike Versus a Bike with Training Wheels
I often tell families ready to progress their children from a tricycle to a bike, to start with a balance bike. A balance bike is simply a bike without pedals where children use their legs instead of pedals to move.
Skip the step of learning with training wheels because children can get dependent on leaning on them for balance. The Balance Bike enables the child to learn to find their center of balance on their own
NOTE: Not everyone will be able to get a balance bike and a bike with training wheels, so I recommend taking the training wheels AND the pedals off of a bike to convert it to a balance bike. A bike shop can help make this adjustment.
Biking with Training Wheels
The problem with a bike with training wheels is the braking system. They use coaster brakes which means pedaling backward to activate the brakes.
Kids tend to start pedaling backward when they encounter resistance which activates the brakes. It’s always difficult for kids with motor planning issues to figure this out. That’s why you ensure they master the pedaling part of bike riding before moving on.

Keep an eye out for the following:
- Some kids tend to push with their legs while pulling on the handlebars, which causes the bikes to turn – as a PT, this signals to me that they need core strengthening
- Some kids will over push with their legs causing them to slip backward on the bike seat – I put a dycem (non-slip pad) or tie a theraband on the seat to prevent this .
Tips to Use a Balance Bike
- Start with having the child walk with their legs while sitting on the saddle. See if they have the control to keep the bike from tipping or even recognize that the bike is tipped while they are riding it. They need to integrate this part. Children with body awareness issues will not even recognize that they are tilted when propelling a balance bike.
- Watch out for kids who walk the bikes, but they are standing and not sitting on the seat. I sometimes use an ace wrap to secure their pelvis on the seat to prevent this
- Once they master keeping the bike upright, work on gliding .
- Gliding – have them take three steps: 1, 2, 3, then bring their feet up to glide. Challenge them and ask them to see how far they can glide before they put their feet down.
- I sometimes use floor markings like chalk on the surface to mark a certain point. Children can work on balancing better if they have a visual cue on how far to glide.
- Once a child can glide for 10-20 feet consistently, I move them to a bike with two wheels (or put the pedals back on the bike).
Steps to Help Children Ride a Standard Bike
- Work in a parking lot of a school or a park early in the morning so that it will be empty and there are no distractions – avoid the sidewalks or narrow spaces because the child needs to worry about staying within the confines of the space (it can become too stressful for them).
- Try to find a parking lot with a little downward incline to help them get a little momentum to balance.
- Let your child walk the bike out to the parking lot while holding the handlebar. This way, they learn to handle the bike and how to motor plan to keep it balanced.
- Work on pedaling forward first. Worry about turns later.
- Have a gait belt (or Dad’s belt) around their trunk, so you have something to grab onto when they are riding (if they are not using a bike with a parent’s handle).
- Give them a little push to start them up – they will usually start slow because they are apprehensive but what children don’t realize yet is they need momentum to be able to balance.
- Give them frequent breaks, and maybe bring a snack, as bike riding can be stressful while learning. Let them know that they have to do 2-3 laps then they can take a break. Break for 1-2 mins, get a drink or snacks, then return to bike riding. Use a timer so they know break time is over when it rings. This way, they may be more cooperative when they know they have a break.
- Once they master going straight, you can work on turning – put cones on each end of the parking lot and ask them to turn around the cones. This way, they can practice tight turns.
- Once they master turning, work on tighter areas (e.g. a hallway, sidewalk) to narrow their space.
- Once they master tight areas, work on going up inclines.
Biking From a Complete Stop
- Determine the child’s balance leg – it’s usually the first leg they put down when they stop.
- Once that’s determined, the balance leg is the leg that will stay on the ground and will be pushing to get the bike going. The other leg goes on the pedal (pedal leg).
- Teach the child to position the pedal (pedal leg side) in front of their shin so they can easily put their foot on it.
- Ask them to have the balance leg push on the ground while the pedal leg is pushing down on the pedal to start the bike .

Cycling Benefits
I hope this blog has been helpful wherever your child is on their cycling journey! Teaching children to cycle has numerous benefits to their development, including improving motor skills, strength and balance. It’s also a fun exercise that can be enjoyed with a sibling or friend!
If you ever have concerns about your child’s mobility, strength, or motor skills, Easterseals DuPage & Fox Valley is here to help! Learn more about our physical therapy services by visiting:
https://www.easterseals.com/dfv/our-programs/medical-rehabilitation/physical-therapy.We also invite your family to join our annual Bike for the Kids in Elgin on August 25, 2024!
Cyclists of all ages and abilities are welcome to come and enjoy routes on the Fox Valley Trail. Adapted bikes and trailers are welcome. All ages and abilities are encouraged to participate.

The event includes games, a taco truck, adapted bike giveaway and more as we share the joy of cycling with children of all abilities.
Learn more and register here:
https://www.classy.org/event/9th-annual-bike-for-the-kids/e583185 -
Enjoy A Summer Full of Sensory Activities!
Tuesday, July 23, 2024, 3:41 PM
By: Easterseals DuPage & Fox Valley Occupational Therapy Department “Summer is a grea…
Read this PostBy: Easterseals DuPage & Fox Valley Occupational Therapy Department
“Summer is a great time to explore a large variety of playful sensory input types for children. From messy play and crafts to outdoor activities, children and families can immerse themselves in expanding their touch, sound, sight and movement-based sensory options,” shares Andrea Sagel, MS, OTR/L, Director of Occupational and Developmental Therapy.
One of the best summer activities is around water play! Here are some ideas of both indoor and outdoor sensory play using the theme of water.
SPLASH INTO SUMMER WITH NEW ACTIVITIES!
Simple activities in the bathtub or going to a splash pad or playground can provide fun opportunities to play while improving a child’s visual processing, hand strength and more!
Water Play!
Walking or running in water increases resistance and helps with awareness.
Crawling on hands and knees in water increases a child’s muscle mobility and strength.
Bath Time Fun!
Suggested items to put together into a bag to play with in the tub/pool to develop hand strength and coordination as well as visual motor skills.
- Use sponges or washcloths to fill- up with water and squeeze them out.
- Fill mist or squeeze bottle up with water and watch the mist appear.
- An eye dropper is a great tool to squeeze picking up water and releasing it into another container.
- Use squirt toys such as traditional water guns or super soakers!
- Traditional squirt guns which need a thumb and index finger to use with a squeezing motion. These develop palm strength.
Messy Boats: Sticky, Yummy Toddler Play!
Let your toddler explore the world around them and learn about their senses with messy activities! Read more about this messy boats activity involving gelatin along with a great clean-up strategy from from Busy Toddler here!

Photo Credit: busytoddler.com Hand-Eye Coordination Activities
These activities enhance motor skills which helps movement in eyes, hands, and feet while performing different tasks. Some of these activities at the playground can involve many different input types, such as visual processing and hand eye-coordination.
Velcro Ball and Mitt Sets!
Simply pulling balls off mitts helps with eye-hand coordination and upper-body strength!
Playground Fun!
Hang on a bar for a count of 3 and increase as your child is able!
On a swing: name a body part, i.e., arms or legs, and have them bring that part forward for you to tickle, push, etc.
ARGH!
Walk the Plank Activity from “Tools to Grow”!
Make a simple balance beam or wood beam 4 inches wide. Walk backwards, forward, and even sideways! Test your balance skills or time how long before you fall off. Set goals and accomplish them.
Find more of these activities’ day by day in the “Tools to Grow” website! The site has daily activities for caregivers to do with kids each day for the summer targeting different areas of cous like visual motor skills. (Level 1 is for Preschool- 1st grade and Level 2 is for 2nd grade – 4th grade.)
Floor is Lava Hopscotch Activity!
To provide a child with increased proprioceptive input, motor planning, tactile processing, and handwriting: try Hopscotch or drawing a “floor is lava” course with chalk. This can be done on the driveway or on the sidewalk. Families can use a hose or spray bottle to spray away the chalk when done!
Photo Credit: http://www.hopscotchin.com

For more summer sensory ideas, or ways to adapt these activities to your child’s needs and goals, ask an occupational therapist at Easterseals DuPage & Fox Valley. For more information about our occupational therapy services, visit our website.
Enjoy your summer!
-
Understanding and Supporting Your Child’s Mental Health
Friday, September 8, 2023, 8:58 AM
By Katelyn Bentel, MSW, LSW Social Worker at Easterseals DuPa…
Read this PostBy Katelyn Bentel, MSW, LSW
Social Worker at Easterseals DuPage & Fox ValleyMental health is at the core of human interaction and is the foundation from which individuals navigate their world. Mental health can be difficult to understand because it does not manifest in the same way across the human population—let alone in an individual on a day-to-day basis. We all respond differently!
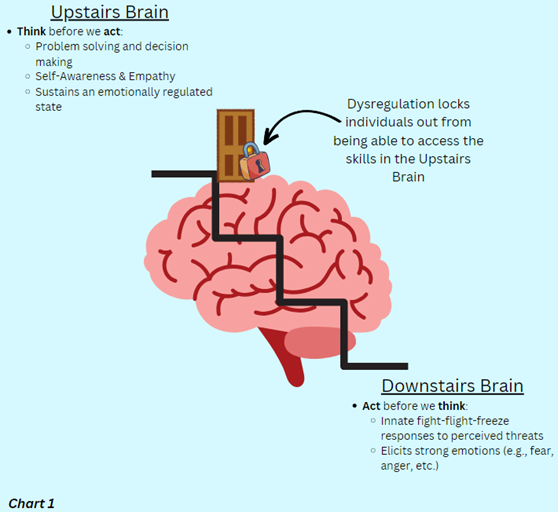
In healthy individuals, the upstairs brain (prefrontal cortex) is fully developed by the age of 25. This part of the brain is responsible for executive functioning skills (e.g., decision-making/impulse control, problem-solving, working memory, attention, emotional regulation, etc.). With this, adults possess an ability to discern emotions and process their own mental distress through self-reflection, which can potentially lead to them seeking out additional support—if deemed necessary.
Children instinctually operate from their downstairs brain (cerebellum, brainstem, and limbic system); responsible for basic, life-sustaining processes (e.g., breathing) and the fight-flight-freeze response in moments of perceived stress/danger.
Their ability to identify, understand, and control their emotions is limited due to an underdeveloped upstairs brain, making it difficult to monitor and communicate struggles with their own mental health, thus, emphasizing the need for extra support.
Signs that your child may need additional support:
- Aggression/increased fighting
- Increased emotional sensitivity
- Frequent temper tantrums/uncharacteristic mood swings
- Stomachaches, headaches, physical complaints
- Loss of interest in previously enjoyed activities/self-isolation
- Inattentiveness
- Difficulty separating from caregivers
- Noticeable change in appetite
- Noticeable decrease in sleep quality
- Lack of self-confidence
These signs can temporarily appear during a child’s typical developmental process as they learn to adjust to inevitable stressors in their environment. However, these signs can also evolve into maladaptive coping skills—negatively impacting the child’s overall mental health. It is important to take notice of the presence of these signs, their frequency, duration, and impact on the child’s ability to function daily.
Understanding why your child is responding this way
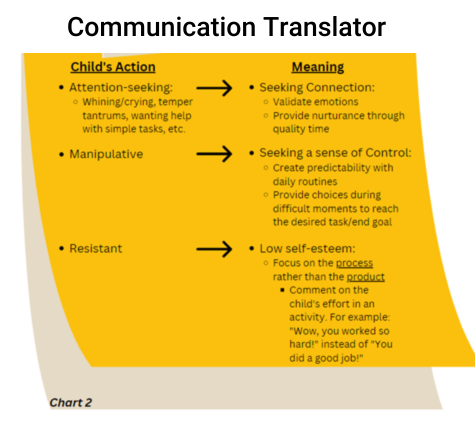
Sometimes a child’s response to stress is misinterpreted as “bad behaviors.” A healthier and more sensitive way to interpret these responses is to reframe “bad behaviors” as communication in an attempt to express an unmet need.
For example, a child may be acting in ways that appear “attention-seeking” (e.g., whining/crying, temper tantrums, wanting help with simple tasks, etc.) when, in reality, they are having difficulty communicating that they are trying to seek out connection.How to respond with Connection:
- Nurturance
· Respect and acknowledge child’s feelings
· Talk and act so child feels seen and safe
· Be Gentle
· Offer affection (verbal or physical)
· Encourage!
· Allow for mistakes
· Be consistent with developmentally appropriate rules and expectations - Validation of emotion
· Respect and acknowledge child’s feelings - Shared quality time with caregiver
· “Special Time,” just you and child
· Include child in your activities
· PLAY!
Another example of a misinterpretation is when a child is viewed as “manipulative” while, in reality, the child could be acting in ways that give them some semblance of control. Children are reliant on their caregivers to have their needs met. This has the potential to come with the repercussion of the child feeling as though they have lost their voice when (well-intentioned) decisions are made on their behalf by caregivers.
This lost voice may make a child feel uneasy, urging them to act in maladaptive ways as a coping mechanism to satisfy that lack of a sense of control. A simple way to instill a child’s sense of control is by offering the child options to choose from to complete the caregiver’s desired task/end goal. These examples are not to be confused as excuses for a child’s behavior or to invalidate a caregiver’s frustration, but rather, to serve as a potential explanation and encourage caregivers to pause and be curious about the why behind these actions. (See Chart 2)Seeking Additional Support
Seeking additional mental health support from a professional is a great use of resources if these dysfunctional responses become a consistent presence in a child’s everyday life. Everyone can benefit from support. For instance, if an individual is recovering from a weakened ankle from a sports injury, it is common to receive physical therapy to rebuild that muscle. We should do the same for someone struggling with emotions or adapting to stressors.
There is no better time to create a strong foundation for mental health and foster resilience than during childhood. The Mental Health & Family Support Team at Easterseals DuPage & Fox Valley provides a safe and inclusive space for children and their families to receive support. Learn more about our mental health services here.
Let's Keep in Touch
Don't miss out on exciting news, helpful resources, and impactful stories delivered to your inbox each month.
Join Today